Are Masks Beneficial?
Masks Are Neither Effective Nor Safe: A Summary Of The Science
Masks Are Neither Effective Nor Safe: A Summary Of The Science
Boat load of noteworthy research:
An overview of the current evidence regarding the effectiveness of face masks.
1. Studies on the effectiveness of face masks
So far, most studies found little to no evidence for the effectiveness of cloth face masks in the general population, neither as personal protective equipment nor as a source control.
- A May 2020 meta-study on pandemic influenza published by the US CDC found that face masks had no effect, neither as personal protective equipment nor as a source control. (Source)
- A Danish randomized controlled trial with 6000 participants, published in the Annals of Internal Medicine in November 2020, found no statistically significant effect of high-quality medical face masks against SARS-CoV-2 infection in a community setting. (Source)
- A large randomized controlled trial with close to 8000 participants, published in October 2020 in PLOS One, found that face masks “did not seem to be effective against laboratory-confirmed viral respiratory infections nor against clinical respiratory infection.” (Source)
- A February 2021 review by the European CDC found no significant evidence supporting the effectiveness of non-medical and medical face masks in the community. Furthermore, the European CDC advised against the use of FFP2/N95 respirators by the general public. (Source)
- A July 2020 review by the Oxford Centre for Evidence-Based Medicine found that there is no evidence for the effectiveness of cloth masks against virus infection or transmission. (Source)
- A November 2020 Cochrane review found that face masks did not reduce influenza-like illness (ILI) cases, neither in the general population nor in health care workers. (Source)
- An April 2020 review by two US professors in respiratory and infectious disease from the University of Illinois concluded that face masks have no effect in everyday life, neither as self-protection nor to protect third parties (so-called source control). (Source)
- An article in the New England Journal of Medicine from May 2020 came to the conclusion that cloth face masks offer little to no protection in everyday life. (Source)
- A 2015 study in the British Medical Journal BMJ Open found that cloth masks were penetrated by 97% of particles and may increase infection risk by retaining moisture or repeated use. (Source)
- An August 2020 review by a German professor in virology, epidemiology and hygiene found that there is no evidence for the effectiveness of cloth face masks and that the improper daily use of masks by the public may in fact lead to an increase in infections. (Source)
An overview:
- A meta-study in the journal Lancet, commissioned by the WHO, claimed that masks “could” lead to a reduction in the risk of infection, but the studies considered mainly N95 respirators in a hospital setting, not cloth masks in a community setting, the strength of the evidence was reported as “low”, and experts found numerous flaws in the study. Professor Peter Jueni, epidemiologist at the University of Toronto, called the WHO study “essentially useless”.
- A study in the journal PNAS claimed that masks had led to a decrease in infections in three global hotspots (including New York City), but the study did not take into account the natural decrease in infections and other simultaneous measures. The study was so flawed that over 40 scientists recommended that the study be withdrawn.
- A US study claimed that US counties with mask mandates had lower Covid infection and hospitalization rates, but the authors had to withdraw their study as infections and hospitalizations increased in many of these counties shortly after the study was published.
- A German study claimed that the introduction of mandatory face masks in German cities had led to a decrease in infections. But the data does not support this claim: in some cities there was no change, in others a decrease, in others an increase in infections (see graph below). The city of Jena was an ‘exception’ only because it simultaneously introduced the strictest quarantine rules in Germany, but the study did not mention this.
- A Canadian study claimed that countries with mandatory masks had fewer deaths than countries without mandatory masks. But the study compared African, Latin American, Asian and Eastern European countries with very different infection rates and population structures.
- A review by the University of Oxford claimed that face masks are effective, but it was based on studies about SARS-1 and in health care settings, not in community settings.
- A review by members of the lobby group ‘Masks for All’, published in the journal PNAS, claimed that masks are effective as a source control against aerosol transmission in the community, but the review provided no real-world evidence supporting this proposition.
2. Zhu JH et al. Effects of long-duration wearing of N95 respirator and surgical facemask: a pilot study. J Lung Pulm Resp Res 2014:4:97-100.
3. Ong JJY et al. Headaches associated with personal protective equipment- A cross-sectional study among frontline healthcare workers during COVID-19. Headache 2020;60(5):864-877.
4. Bader A et al. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia 2008;19:12-126.
5. Shehade H et al. Cutting edge: Hypoxia-Inducible Factor-1 negatively regulates Th1 function. J Immunol 2015;195:1372-1376.
6. Westendorf AM et al. Hypoxia enhances immunosuppression by inhibiting CD4+ effector T cell function and promoting Treg activity. Cell Physiol Biochem 2017;41:1271-84.
7. Sceneay J et al. Hypoxia-driven immunosuppression contributes to the pre-metastatic niche. Oncoimmunology 2013;2:1 e22355.
8. Blaylock RL. Immunoexcitatory mechanisms in glioma proliferation, invasion and occasional metastasis. Surg Neurol Inter 2013;4:15.
Do facemasks protect against COVID‐19?
"A meta‐analysis of randomised controlled trials of pre‐COVID‐19 showed that surgical masks or N95 respirators reduced clinical respiratory illness in health‐care workers by 41% and influenza‐like illness by 66%: they work but are far from perfect. 1 N95 masks were not statistically better than surgical masks in preventing proven influenza, 2 nor in preventing COVID‐19, although the latter is based on weak data. 3 N95 masks are more efficient filters of small particles, but these findings suggest it is reasonable to recommend that health‐care workers use surgical masks when there is risk of droplet spread and reserve precious N95 masks for health‐care workers performing aerosol‐generating procedures."
"The public might wear masks to avoid infection or to protect others. During the 2009 pandemic of H1N1 influenza (swine flu), encouraging the public to wash their hands reduced the incidence of infection significantly whereas wearing facemasks did not. 5There is no good evidence that facemasks protect the public against infection with respiratory viruses, including COVID‐19. 6"
"During the pandemics caused by swine flu and by the coronaviruses which caused SARS and MERS, many people in Asia and elsewhere walked around wearing surgical or homemade cotton masks to protect themselves. One danger of doing this is the illusion of protection. Surgical facemasks are designed to be discarded after single use. As they become moist they become porous and no longer protect. Indeed, experiments have shown that surgical and cotton masks do not trap the SARS‐CoV‐2 (COVID‐19) virus, which can be detected on the outer surface of the masks for up to 7 days. 7 , 8 Thus, a pre‐symptomatic or mildly infected person wearing a facemask for hours without changing it and without washing hands every time they touched the mask could paradoxically increase the risk of infecting others. Because the USA is in a desperate situation, their Centers for Disease Control has recommended the public wear homemade cloth masks. This was essentially done in an effort to try and reduce community transmission, especially from people who may not perceive themselves to be symptomatic, rather than to protect the wearer, although the evidence for this is scant. In contrast, the World Health Organization currently recommends against the public routinely wearing facemasks.In Australia and New Zealand currently, the questionable benefits arguably do not justify health‐care staff wearing surgical masks when treating low‐risk patients and may impede the normal caring relationship between patients, parents and staff. We counsel against such practice, at least at present."
Volume 26, Number 5—May 2020
Policy Review
Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures
https://pubmed.ncbi.nlm.nih.gov/18500410/
https://pubmed.ncbi.nlm.nih.gov/15340662/
https://clinicaltrials.gov/ct2/show/NCT00173017
https://pubmed.ncbi.nlm.nih.gov/18331781/
https://www.nature.com/articles/s41598-018-35797-3
https://pubmed.ncbi.nlm.nih.gov/31479137/
https://bmjopen.bmj.com/content/5/4/e006577#T1
https://pubmed.ncbi.nlm.nih.gov/21477136/
https://pubmed.ncbi.nlm.nih.gov/28039289/
https://bmjopen.bmj.com/content/5/4/e006577.long
https://pubmed.ncbi.nlm.nih.gov/20584862/
https://pubmed.ncbi.nlm.nih.gov/22188875/
https://pubmed.ncbi.nlm.nih.gov/31479137/
https://pubmed.ncbi.nlm.nih.gov/27531371/
https://pubmed.ncbi.nlm.nih.gov/29855107/
https://pubmed.ncbi.nlm.nih.gov/29678452/
https://pubmed.ncbi.nlm.nih.gov/25806411/
https://pubmed.ncbi.nlm.nih.gov/23108786/
https://pubmed.ncbi.nlm.nih.gov/25858901/
https://pubmed.ncbi.nlm.nih.gov/5333967/
https://journals.plos.org/plosone/article…
https://academic.oup.com/annweh/article/54/7/789/202744
https://pubmed.ncbi.nlm.nih.gov/27531371/
https://www.nature.com/articles/s41591-020-0843-2
https://vimeo.com/424254660
https://www.facebook.com/watch/live/?v=276231940292992&ref=watch_permalink
https://www.youtube.com/watch?v=D0t84p6H4XA
https://pubmed.ncbi.nlm.nih.gov/19216002/
https://www.cambridge.org/…/64D368496EBDE0AFCC6639CCC9D8BC05
https://onlinelibrary.wiley.com/…/…/j.1750-2659.2011.00307.x
https://www.cmaj.ca/content/188/8/567
https://academic.oup.com/cid/article/65/11/1934/4068747
https://jamanetwork.com/journals/jama/fullarticle/2749214
https://onlinelibrary.wiley.com/doi/epdf/10.1111/jebm.12381
https://citeseerx.ist.psu.edu/viewdoc/download…
https://www.cambridge.org/…/0921A05A69A9419C862FA2F35F819D55
https://academic.oup.com/cid/article/11/3/494/397025
https://royalsocietypublishing.org/d…/10.1098/rsif.2011.0537
https://journals.plos.org/plosone/article…
https://bmcpublichealth.biomedcentral.com/…/1471-2458-12-106
https://royalsocietypublishing.org/d…/10.1098/rsif.2010.0686
https://link.springer.com/article/10.1007/s12560-011-9056-7
• Jacobs, J. L. et al. (2009) "Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: A randomized controlled trial," American Journal of Infection Control, Volume 37, Issue 5, 417 - 419.
N95-masked health-care workers (HCW) were significantly more likely to experience headaches. Face mask use in HCW was not demonstrated to provide benefit in terms of cold symptoms or getting colds.
None of the studies reviewed showed the benefit of wearing a mask in either HCW or community members in households (H). See summary Tables 1 and 2 therein.
• Do used and loaded masks become sources of enhanced transmission, for the wearer and others?
• Do masks become collectors and retainers of pathogens that the mask wearer would otherwise avoid when breathing without a mask?
• Are large droplets captured by a mask atomized or aerosolized into breathable components? Can virions escape an evaporating droplet stuck to a mask fiber?
• What are the dangers of bacterial growth on a used and loaded mask?
• How do pathogen-laden droplets interact with environmental dust and aerosols captured on the mask?
• What are long-term health effects on HCW, such as headaches, arising from impeded breathing?
• Are there negative social consequences to a masked society?
• Are there negative psychological consequences of wearing a mask, as a fear-based behavioral modification?
• What are the environmental consequences of mask manufacturing and disposal?
• Do the masks shed fibers or substances that are harmful when inhaled?
God bless y’all Dr. Serge
Thinking a mask will save you is like thinking a 'filter' on a cigarette will prevent lung cancer.
Volume 26, Number 5—May 2020
Policy Review
Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures
Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings-International Travel-Related Measures
Now that we have a randomized controlled trial (RCT) about masks, will it change what you do?
Mask Facts
Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—International Travel-Related Measures
Sukhyun Ryu, Huizhi Gao, [...], and Benjamin J. Cowling
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7181936/
From the CDC:::
Community and Close Contact Exposures Associated with COVID-19 Among Symptomatic Adults ≥18 Years in 11 Outpatient Health Care Facilities — United States, July 2020
https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6936a5-H.pdf?fbclid=IwAR2oybbWzTy8HckcGsZRidy4N1ylf7Tp5hP2MyapiLO8dMu1Y_cYkhLqrcg
Mask Facts
https://aapsonline.org/mask-facts/?fbclid=IwAR1Pl-aVBH6O1qo_XwRPXSSQHUeBW0J6xtBaMOjiykPIL5_om95v4vc2Pcs- Virus is transmitted through respiratory droplets produced when an infected person coughs, sneezes or talks. Larger respiratory droplets (>5 μm) remain in the air for only a short time and travel only short distances, generally <1 meter. They fall to the ground quickly. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30245-9/fulltext
- This idea guides the CDC’s advice to maintain at least a 6-foot distance.
- Virus-laden small (<5 μm) aerosolized droplets can remain in the air for at least 3 hours and travel long distances. https://www.nejm.org/doi/pdf/10.1056/NEJMc2004973?articleTools=true
- In air conditioned environment these large droplets may travel farther.
- However, ventilation — even the opening of an entrance door and a small window can dilute the number of small droplets to one half after 30 seconds. (This study looked at droplets from uninfected persons). This is clinically relevant because poorly ventilated and populated spaces, like public transport and nursing homes, have high SARS-CoV-2 disease transmission despite physical distancing. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30245-9/fulltext
- Person to person touching
- The CDC’s most recent statement regarding contracting COVID-19 from touching surfaces: “Based on data from lab studies on Covid-19 and what we know about similar respiratory diseases, it may be possible that a person can get Covid-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose or possibly their eyes,” the agency wrote. “But this isn’t thought to be the main way the virus spreads. https://www.cdc.gov/media/releases/2020/s0522-cdc-updates-covid-transmission.html.
- Chinese study with data taken from swabs on surfaces around the hospital
https://wwwnc.cdc.gov/eid/article/26/7/20-0885_article?deliveryName=USCDC_333-DM25707- The surfaces where tested with the PCR (polymerase chain reaction) test, which greatly amplifies the viral genetic material if it is present. That material is detectable when a person is actively infected. This is thought to be the most reliable test.
- Computer mouse (ICU 6/8, 75%; General ward (GW) 1/5, 20%)
- Trash cans (ICU 3/5, 60%; GW 0/8)
- Sickbed handrails (ICU 6/14, 42.9%; GW 0/12)
- Doorknobs (GW 1/12, 8.3%)
- 81.3% of the miscellaneous personal items were positive:
- Exercise equipment
- Medical equipment (spirometer, pulse oximeter, nasal cannula)
- PC and iPads
- Reading glasses
- Cellular phones (83.3% positive for viral RNA)
- Remote controls for in-room TVs (64.7% percent positive)
- Toilets (81.0% positive)
- Room surfaces (80.4% of all sampled)
- Bedside tables and bed rails (75.0%)
- Window ledges (81.8%)
- Plastic: up to 2-3 days
- Stainless Steel: up to 2-3 days
- Cardboard: up to 1 day
- Copper: up to 4 hours
- Floor – gravity causes droplets to fall to the floor. Half of ICU workers all had virus on the bottoms of their shoes
- The surfaces where tested with the PCR (polymerase chain reaction) test, which greatly amplifies the viral genetic material if it is present. That material is detectable when a person is actively infected. This is thought to be the most reliable test.
- HEPA (high efficiency particulate air) filters – 99.97 – 100% efficient. HEPA filters are tested with particles that are 0.125 μm.
- Masks and respirators work by collecting particles through several physical mechanisms, including diffusion (small particles) and interception and impaction (large particles)
- N95 filtering facepiece respirators (FFRs) are constructed from electret (a dielectric material that has a quasi-permanent electric charge. An electret generates internal and external electric fields so the filter material has electrostatic attraction for additional collection of all particle sizes. As flow increases, particles will be collected less efficiently.
- N95 – A properly fitted N95 will block 95% of tiny air particles down to 0.3 μm from reaching the wearer’s face. https://www.honeywell.com/en-us/newsroom/news/2020/03/n95-masks-explained.
- But even these have problems: many have exhalation valve for easier breathing and less moisture inside the mask.
- Surgical masks are designed to protect patients from a surgeon’s respiratory droplets, aren’t effective at blocking particles smaller than 100 μm. https://webcache.googleusercontent.com/search?q=cache:VLXWeZBll7YJ:https://multimedia.3m.com/mws/media/957730O/respirators-and-surgical-masks-contrast-technical-bulletin.pdf+&cd=13&hl=en&ct=clnk&gl=us
- Filter efficiency was measured across a wide range of small particle sizes (0.02 to 1 µm) at 33 and 99 L/min.
- N95 respirators had efficiencies greater than 95% (as expected).
- T-shirts had 10% efficiency,
- Scarves 10% to 20%,
- Cloth masks 10% to 30%,
- Sweatshirts 20% to 40%, and
- Towels 40%.
- All of the cloth masks and materials had near zero efficiency at 0.3 µm, a particle size that easily penetrates into the lungs.
- Another study evaluated 44 masks, respirators, and other materials with similar methods and small aerosols (0.08 and 0.22 µm).
- N95 FFR filter efficiency was greater than 95%.
- Medical masks – 55% efficiency
- General masks – 38% and
- Handkerchiefs – 2% (one layer) to 13% (four layers) efficiency.
- Conclusion: Wearing masks will not reduce SARS-CoV-2.
- N95 masks protect health care workers, but are not recommended for source control transmission.
- Surgical masks are better than cloth but not very efficient at preventing emissions from infected patients.
- Cloth masks will be ineffective at preventing SARS-CoV-2 transmission, whether worn as source control or as personal protective equipment (PPE).
- Penetration of cloth masks by particles was 97% and medical masks 44%, 3M Vflex 9105 N95 (0.1%), 3M 9320 N95 (<0.01%).
- Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection.
- The virus may survive on the surface of the face- masks
- Self-contamination through repeated use and improper doffing is possible. A contaminated cloth mask may transfer pathogen from the mask to the bare hands of the wearer.
- Cloth masks should not be recommended for health care workers, particularly in high-risk situations, and guidelines need to be updated.
- cover their nose and mouth when coughing or sneezing,
- use tissues to contain respiratory secretions and, after use, to dispose of them in the nearest waste receptacle, and
- perform hand hygiene (e.g., handwashing with non-antimicrobial soap and water, and alcohol-based hand rub if soap and water are not available) after having contact with respiratory secretions and contaminated objects/materials.
- Surgical masks – loose fitting. They are designed to protect the patient from the doctors’ respiratory droplets. The wearer is not protected from others airborne particles
- People do not wear masks properly. Most people have the mask under the nose. The wearer does not have glasses on and the eyes are a portal of entry.
- The designer masks and scarves offer minimal protection – they give a false sense of security to both the wearer and those around the wearer.
**Not to mention they add a perverse lightheartedness to the situation. - If you are walking alone, no mask – avoid folks – that is common sense.
- Remember – children under 2 should not wear masks – accidental suffocation and difficulty breathing in some
- If wearing a mask makes people go out and get Vitamin D – go for it. In the 1918 flu pandemic people who went outside did better. Early reports are showing people with COVID-19 with low Vitamin D do worse than those with normal levels. Perhaps that is why shut-ins do so poorly. https://www.medrxiv.org/content/10.1101/2020.04.08.20058578v4
Sums things up nicely
Ben Swann
https://www.facebook.com/BenSwannRealityCheck/videos/705845830268772/
Evidence Not FEar
https://evidencenotfear.com/tag/face-masks/
The truth about face masks and the coronavirus: Wearing masks in crowded places may help reduce the spread, but it isn't a perfect solution
The Use of Masks and Respirators to Prevent Transmission of Influenza: A Systematic Review of the Scientific Evidence
Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis
CONCLUSION:
"The use of N95 respirators compared with surgical masks is not associated with a lower risk of laboratory-confirmed influenza. It suggests that N95 respirators should not be recommended for general public and nonhigh-risk medical staff those are not in close contact with influenza patients or suspected patients."
WHO says there is no need for healthy people to wear face masks, days after the CDC told all Americans to cover their faces
Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients
Identifying airborne transmission as the dominant route for the spread of COVID-19
A cluster randomised trial of cloth masks compared with medical masks in healthcare workers
Conclusions
This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally.
"The use of cloth masks is widespread around the world, particularly in countries at high-risk for emerging infections, but there have been no efficacy studies to underpin their use."
Sequential CQ / HCQ Research Papers and Reports
Mask Hysteria: Are We Going Too Far?
— Kevin Campbell believes media and politicians use masking as a way to fear monger
Here are 12 FACTS that we KNOW…
- No studies have been done to demonstrate that either a cloth mask or the N95 mask has any effect on transmission of COVID-19. As a matter of fact, research published in the Annals of Internal Medicine at the first of April indicated that “both surgical and cotton masks seem to be ineffective in preventing the dissemination of SARS–CoV-2 from the coughs of patients with COVID-19.” (Reference)
- In a February 2020 meta-analysis of six randomized controlled trials involving 9,171 patients, there were no statistically significant differences in preventing influenza or viral infections using N95 respirators and surgical masks. (Reference)
- A May 2020 study involving 159 healthcare workers aged 21 to 35 years of age found that 81% developed headaches from wearing a face mask. (Reference)
- In a 2008 study of surgical masks worn by 53 surgeons, researchers found that the mask reduced the blood oxygen levels significantly, creating a condition known as “hypoxia.” (Reference)
- A 2015 study indicated that hypoxia inhibits T-lymphocytes (the main immune cells used to fight viral infections) by increasing the level of a compound called hypoxia inducible factor-1 (HIF-1). (Reference) In other words, wearing a mask, which has been shown to cause hypoxia, may actually set the stage for contracting COVID-19 and make the consequences much worse.
- Hypoxia promotes inflammation which can promote the growth, invasion and spread of cancers. (Reference) Hypoxia is also a significant factor in atherosclerosis, thus it increases the risk of stroke and heart attack. (Reference)
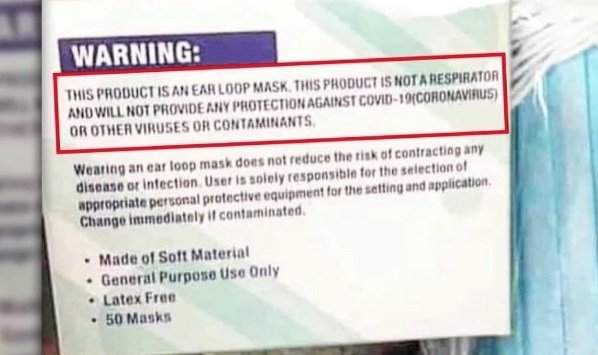
- The WARNING on the box of surgical masks states clearly “THIS PRODUCT WILL NOT PROVIDE ANY PROTECTION AGAINST COVID-19 (CORONAVIRUS) OR OTHER VIRUSES OR CONTAMINANTS.”
- Those who wear masks are constantly rebreathing the viruses, raising the concentration of the virus in the lungs and the nasal passages. By wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, enter the olfactory nerves and can travel into the brain. (Reference, Reference, Reference)
- Anthony Fauci, head of the director of the National Institute of Allergy and Infectious Diseases (NIAID), did an interview on 60 Minutes where he said, “People shouldn’t be walking around wearing masks.”
- The World Health Organization says that there is no need for healthy people to wear face masks. (Reference) They recommend that healthy people only wear masks when taking care of someone infected with COVID-19. (Reference)
- Surgeon General Jerome Adams advised against the general public wearing face masks, saying they were “not proven to be effective” in preventing people from contracting COVID-19. (Reference)
- Although the CDC recommends wearing masks, they admitted that they do not have data to confirm that wearing a mask reduces the risk of contracting or spreading COVID-19. (Reference)
Blaylock: Face Masks Pose Serious Risks To The Healthy
Shelby Co. Health Dept. stops distribution of face masks over health concerns

Face masks should be used only by individuals who have symptoms of respiratory infection such as coughing, sneezing, or, in some cases, fever. Face masks should also be worn by health care workers, by individuals who are taking care of or are in close contact with people who have respiratory infections, or otherwise as directed by a doctor. Face masks should not be worn by healthy individuals to protect themselves from acquiring respiratory infection because there is no evidence to suggest that face masks worn by healthy individuals are effective in preventing people from becoming ill. Face masks should be reserved for those who need them because masks can be in short supply during periods of widespread respiratory infection. Because N95 respirators require special fit testing, they are not recommended for use by the general public.
Compilation of Research
From Dr. Brett Jones
https://docs.google.com/document/d/1DCEjDgnEqW4GMBYUshXWgR_lO6H583iOYYFJjyCaytU/edit?fbclid=IwAR3NaYtn1NF5oJ0OomBDkO4Tj_9hM5T5eN1vvLxirRNO-S27aju7jKcONgc
The US Surgeon General once warned against wearing face masks for the coronavirus but the CDC now recommends it
https://www.businessinsider.com/americans-dont-need-masks-pence-says-as-demand-increases-2020-2?fbclid=IwAR3L5kYm-YI9OuPumpyTJPxkDVCscHZeaK-bnklG3O3TUo-w1LxOEhszfGwhttps://standforhealthfreedom.com/action/act-now-mandatory-masks-endanger-your-health/
References
1 T Jefferson, M Jones, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. MedRxiv. 2020 Apr 7.
https://www.medrxiv.org/content/10.1101/2020.03.30.20047217v2
2 J Xiao, E Shiu, et al. Nonpharmaceutical measures for pandemic influenza in non-healthcare settings – personal protective and environmental measures. Centers for Disease Control. 26(5); 2020 May.
https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
3 J Brainard, N Jones, et al. Facemasks and similar barriers to prevent respiratory illness such as COVID19: A rapid systematic review. MedRxiv. 2020 Apr 1.
https://www.medrxiv.org/content/10.1101/2020.04.01.20049528v1.full.pdf
4 L Radonovich M Simberkoff, et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinic trial. JAMA. 2019 Sep 3. 322(9): 824-833.
https://jamanetwork.com/journals/jama/fullarticle/2749214
5 J Smith, C MacDougall. CMAJ. 2016 May 17. 188(8); 567-574.
https://www.cmaj.ca/content/188/8/567
6 F bin-Reza, V Lopez, et al. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence. 2012 Jul; 6(4): 257-267.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779801/
7 J Jacobs, S Ohde, et al. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am J Infect Control. 2009 Jun; 37(5): 417-419.
https://pubmed.ncbi.nlm.nih.gov/19216002/
8 M Viola, B Peterson, et al. Face coverings, aerosol dispersion and mitigation of virus transmission risk.
https://arxiv.org/abs/2005.10720, https://arxiv.org/ftp/arxiv/papers/2005/2005.10720.pdf
9 S Grinshpun, H Haruta, et al. Performance of an N95 filtering facepiece particular respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Env Hygiene. 2009; 6(10):593-603.
https://www.tandfonline.com/doi/pdf/10.1080/15459620903120086
10 H Jung, J Kim, et al. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual Res. 2013 Jun. 14:991-1002.
https://aaqr.org/articles/aaqr-13-06-oa-0201.pdf
11 C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577.long
12 N95 masks explained. https://www.honeywell.com/en-us/newsroom/news/2020/03/n95-masks-explained
13 V Offeddu, C Yung, et al. Effectiveness of masks and respirators against infections in healthcare workers: A systematic review and meta-analysis. Clin Inf Dis. 65(11), 2017 Dec 1; 1934-1942.
https://academic.oup.com/cid/article/65/11/1934/4068747
14 C MacIntyre, Q Wang, et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza J. 2010 Dec 3.
15 M Walker. Study casts doubt on N95 masks for the public. MedPage Today. 2020 May 20.
https://www.medpagetoday.com/infectiousdisease/publichealth/86601
16 C MacIntyre, Q Wang, et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza J. 2010 Dec 3.
17 N Shimasaki, A Okaue, et al. Comparison of the filter efficiency of medical nonwoven fabrics against three different microbe aerosols. Biocontrol Sci. 2018; 23(2). 61-69.
https://www.jstage.jst.go.jp/article/bio/23/2/23_61/_pdf/-char/en
18 T Tunevall. Postoperative wound infections and surgical face masks: A controlled study. World J Surg. 1991 May; 15: 383-387.
https://link.springer.com/article/10.1007%2FBF01658736
19 N Orr. Is a mask necessary in the operating theatre? Ann Royal Coll Surg Eng 1981: 63: 390-392.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2493952/pdf/annrcse01509-0009.pdf
20 N Mitchell, S Hunt. Surgical face masks in modern operating rooms – a costly and unnecessary ritual? J Hosp Infection. 18(3); 1991 Jul 1. 239-242.
https://www.journalofhospitalinfection.com/article/0195-6701(91)90148-2/pdf
21 C DaZhou, P Sivathondan, et al. Unmasking the surgeons: the evidence base behind the use of facemasks in surgery. JR Soc Med. 2015 Jun; 108(6): 223-228.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480558/
22 L Brosseau, M Sietsema. Commentary: Masks for all for Covid-19 not based on sound data. U Minn Ctr Inf Dis Res Pol. 2020 Apr 1.
23 N Leung, D Chu, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks Nature Research. 2020 Mar 7. 26,676-680 (2020).
https://www.researchsquare.com/article/rs-16836/v1
24 S Rengasamy, B Eimer, et al. Simple respiratory protection – evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010 Oct; 54(7): 789-798.
https://academic.oup.com/annweh/article/54/7/789/202744
25 S Bae, M Kim, et al. Effectiveness of surgical and cotton masks in blocking SARS-CoV-2: A controlled comparison in 4 patients. Ann Int Med. 2020 Apr 6.
https://www.acpjournals.org/doi/10.7326/M20-1342
26 S Rengasamy, B Eimer, et al. Simple respiratory protection – evaluation of the filtration performance of cloth masks and common fabric materials against 20-1000 nm size particles. Ann Occup Hyg. 2010 Oct; 54(7): 789-798.
https://academic.oup.com/annweh/article/54/7/789/202744
27 C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577.long
28 W Kellogg. An experimental study of the efficacy of gauze face masks. Am J Pub Health. 1920. 34-42.
https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.10.1.34
29 M Klompas, C Morris, et al. Universal masking in hospitals in the Covid-19 era. N Eng J Med. 2020; 382 e63.
https://www.nejm.org/doi/full/10.1056/NEJMp2006372
30 E Person, C Lemercier et al. Effect of a surgical mask on six minute walking distance. Rev Mal Respir. 2018 Mar; 35(3):264-268.
https://pubmed.ncbi.nlm.nih.gov/29395560/
31 B Chandrasekaran, S Fernandes. Exercise with facemask; are we handling a devil’s sword – a physiological hypothesis. Med Hypothese. 2020 Jun 22. 144:110002.
https://pubmed.ncbi.nlm.nih.gov/32590322/
32 P Shuang Ye Tong, A Sugam Kale, et al. Respiratory consequences of N95-type mask usage in pregnant healthcare workers – A controlled clinical study. Antimicrob Resist Infect Control. 2015 Nov 16; 4:48.
https://pubmed.ncbi.nlm.nih.gov/26579222/
33 T Kao, K Huang, et al. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004 Aug; 103(8):624-628.
https://pubmed.ncbi.nlm.nih.gov/15340662/
34 F Blachere, W Lindsley et al. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J Viro Methods. 2018 Oct; 260:98-106.
https://pubmed.ncbi.nlm.nih.gov/30029810/
35 A Rule, O Apau, et al. Healthcare personnel exposure in an emergency department during influenza season. PLoS One. 2018 Aug 31; 13(8): e0203223.
https://pubmed.ncbi.nlm.nih.gov/30169507/
36 F Blachere, W Lindsley et al. Assessment of influenza virus exposure and recovery from contaminated surgical masks and N95 respirators. J Viro Methods. 2018 Oct; 260:98-106.
https://pubmed.ncbi.nlm.nih.gov/30029810/
37 A Chughtai, S Stelzer-Braid, et al. Contamination by respiratory viruses on our surface of medical masks used by hospital healthcare workers. BMC Infect Dis. 2019 Jun 3; 19(1): 491.
https://pubmed.ncbi.nlm.nih.gov/31159777/
38 L Zhiqing, C Yongyun, et al. J Orthop Translat. 2018 Jun 27; 14:57-62.
https://pubmed.ncbi.nlm.nih.gov/30035033/
39 C MacIntyre, H Seale, et al. A cluster randomized trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4)
https://bmjopen.bmj.com/content/5/4/e006577
40 A Beder, U Buyukkocak, et al. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia. 2008; 19: 121-126.
http://scielo.isciii.es/pdf/neuro/v19n2/3.pdf
41 D Lukashev, B Klebanov, et al. Cutting edge: Hypoxia-inducible factor 1-alpha and its activation-inducible short isoform negatively regulate functions of CD4+ and CD8+ T lymphocytes. J Immunol. 2006 Oct 15; 177(8) 4962-4965.
https://www.jimmunol.org/content/177/8/4962
42 A Sant, A McMichael. Revealing the role of CD4+ T-cells in viral immunity. J Exper Med. 2012 Jun 30; 209(8):1391-1395.


Comments